Hemispherectomy
Hemispherectomy is a surgical treatment for epilepsy. In this procedure, one of the two cerebral hemispheres, which make up the majority of the human brain, is removed. There are generally many surgical procedures which can fall under the broad category of hemispherectomy.
The main goal of each procedure is to completely stop seizures by disconnecting one cerebral hemisphere from the other completely. This can prevent seizures from spreading to any other parts of the brain.
Purpose
This surgery is considered when epilepsy cannot be controlled easily by medications. Removing an entire hemisphere of the brain is generally considered an effective treatment, as the removed hemisphere is generally quite damaged by the effects of seizures. In addition, the other brain has already assumed many of the functions of the damaged side. The brain has many redundant systems, allowing healthy regions to make up for the loss of a damaged side.
Children can also be candidates for this procedure; children who usually show significant impairments due to their epilepsy, which can include partial or complete loss of sensation, partial or complete paralysis, or complete loss of sensation on the side of the body opposite to the affected brain region.
Preparation
To be considered a candidate for this procedure, first, you will need to undergo various tests, which can include electroencephalography, in which electrodes are placed on the scalp, on the surface of the brain, or within the brain to record electrical activity. This test helps in locating the focal points of the seizure activity.
Several neuroimaging procedures are also used for obtaining images of the brain, as these can help to reveal structural abnormalities that the neurosurgeon must be aware of. These procedures may include computed tomography (CT) scans, magnetic resonance imaging (MRI), x rays, or positron emission tomography (PET) imaging.
Neuropsychological tests might be done for providing a baseline against which the results of the surgery can be measured. A Wada test may be performed as well. In this test, a drug is injected into the artery putting one half of the brain to sleep. This can help the neurologist to determine where in the brain the language and other functions are localized. This might also be useful for predicting the result of the surgery.
Procedure
Hemispherectomy can be ‘anatomical’ or ‘functional’. In an anatomical hemispherectomy, a hemisphere is removed completely, while in a functional hemispherectomy, some of the tissues are left in place. However, its connection to the other brain is cut so that it is no longer able to function. Anatomic hemispherectomy is also of several types, which are designed to minimize complications.
Generally, most surgical centers prefer to perform functional hemispherectomy. First, the doctor will put you into sleep with general anesthesia.
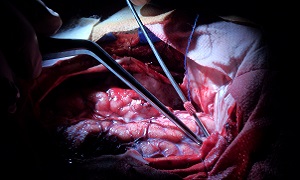
The doctor will next make a cut in your scalp, after which a piece of bone from your skull will be taken out. He/she will move aside part of the dura, a tough membrane covering your brain. Then your doctor will take out parts of the hemisphere where your seizures start. Generally, it is the temporal lobe.
Finally, your doctor will cut the corpus callosum so the hemispheres of your brain are not able to send signals to each other anymore. This way, if there is a seizure in the hemisphere that doesn’t work properly, it will not spread to the healthy one. This will allow the healthy hemisphere to continue to develop in a proper way without the danger of damage by seizures.
Once the surgery is finished, your doctor will be putting the dura and bone back, and then close up the wound with stitches or staples.
Aftercare & recovery
You will be in intensive care for a day or two. Then you will spend a few days in a regular hospital room. The stitches or staples should come out around two weeks after the surgery.
You might experience some side effects in the first few weeks, though these should usually go away within a short time.
- Headaches
- Trouble concentrating
- Trouble finding the right words
- Forgetfulness
- Feeling tired
- Nausea
- Numbness in the scalp
- Feeling depressed
- Puffy eyes
- Muscle weakness on one side of your body
Generally, you should be able to resume your daily activities within 6 to 8 weeks after the surgery. It is likely that you will need to keep taking your seizure medication for at least 2 years, even if you don’t have any seizures. Your doctor will let you know when you need to lower the dose or stop taking it completely.
Risks
Like most major surgeries, there is a risk of infection, bleeding, or allergic reaction to the anesthesia.
Other problems that might occur include:
- Loss of feeling or movement on the opposite side of your body
- Loss of visual field
- Fluid on your brain which can require a second procedure, such as a VP shunt
In around 70-85 percent of patients, seizures are eliminated. In around 10-20 percent of patients, it is reduced by 80 percent. Patients who suffer from Rasmussen disease, which is progressive, might not receive many benefits, though medications can be reduced and there might be some improvement in intellectual function.
Death is also a possibility, though it is known to occur in only 1-2 percent of patients, who undergo hemispherectomy.