Osteomyelitis
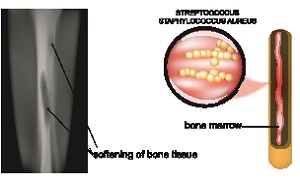
Osteomyelitis is an infection in a bone, which is rare but can be quite serious. Infections reach a bone by spreading from nearby tissue or by traveling through the bloodstream. Infections can also begin in the bone itself, if due to an injury the bone is exposed to germs.
Smokers and people who are suffering from chronic health conditions, like diabetes or kidney failure, are generally more at risk of developing this condition. People having diabetes may develop osteomyelitis in their feet if they have foot ulcers.
Although this condition was once considered incurable, due to advances in modern science and medicine, it can be successfully treated now.
Symptoms
If you are having osteomyelitis, you might show the following signs and symptoms:
- Fever
- Pain in the area of the infection
- Fatigue
- Swelling, warmth, and redness over the area of the infection
Sometimes osteomyelitis doesn’t cause any signs or symptoms or in some cases, they may be hard to distinguish from other problems. This can be true for infants, older adults as well as people with compromised immune systems.
If you ever experience worsening bone pain along with fever, you should see your doctor. If you’re at a risk of infection because of any medical condition or an injury, or recent surgery, you should see your doctor immediately if you notice any signs and symptoms of an infection.
Causes & risk factors
In most cases, a bacteria which is known as Staphylococcus auerus, a type of staph bacteria is known to be the cause of this condition.
Certain chronic conditions such as diabetes can also increase your risk of osteomyelitis.
This condition occurs in only 2 out of every 10,000 people. The condition can affect children as well as adults, although in different ways. Certain conditions or behaviors that can cause the immune system to weaken, can increase the risk of osteomyelitis. These include the following:
- Diabetes
- Sickle cell disease
- Alcoholism
- Long-term use of steroids
- Poor blood supply
- Recent injury
- HIV or AIDS
- Rheumatoid arthritis
- Intravenous drug use
- Hemodialysis
Bone surgery, which includes hip or knee replacements, can also increase the chances of bone infection.
Diagnosis
Your doctor will first likely feel the area around the affected bone for any tenderness, warmth, or swelling. If you are having a foot ulcer, your doctor might use a dull probe in order to determine the proximity of the underlying bone.
Your doctor might also order a combination of tests and procedures in order to diagnose osteomyelitis as well as to determine exactly which germ is causing the infection. Some other tests can include the following:
Blood tests
Blood tests might also reveal any elevated levels of white blood cells as well as other factors which can indicate that your body is combating an infection. If your osteomyelitis is the result of any infection in the blood, tests may reveal which germs are causing it.
However, a blood test will not tell your doctor whether you do or don’t have osteomyelitis. Though, it can give clues to help your doctor decide what additional tests and procedures you are going to require.
Imaging tests
X-rays
Magnetic resonance imaging (MRI)
Computerized tomography (CT)
Bone biopsy
A bone biopsy can help to reveal what type of germ has infected your bone. Knowing the type of germ can help your doctor in choosing an antibiotic that works particularly for that type of infection.
An open biopsy will require anesthesia as well as surgery for accessing the bone. In certain situations, a surgeon may insert a long needle through your skin and into your bone in order to take a biopsy. This procedure will require local anesthetics in order to numb the area where the needle will be inserted. X-ray or other imaging scans might also be used for proper guidance.
Treatment
In many cases, antibiotics and pain medications are able to treat osteomyelitis effectively. If a doctor obtains a biopsy, this will also aid in guiding the choice of the best antibiotic. The duration of treatment of this condition with antibiotics is generally four to eight weeks though it varies with the type of infection as well as the response to the treatments. In few cases, the doctor will need to immobilize an affected area using a brace in order to prevent any pain and speed up the treatment.
Sometimes surgery can become necessary. If there is an area of localized bacteria or joint infection, your doctor might need to open, wash as well as drain it. If there is damaged soft tissue or bone, it might require to be removed as well. If bone removal becomes necessary, it might need to be replaced with a bone graft.
Complications
Complications of this condition can include the following:
- Bone death (osteonecrosis)- An infection in your bone may impede blood circulation within the bone, which might eventually result in bone death. Areas of the body where the bone has died can require surgical removal for any antibiotics to be effective.
- Skin cancer– If your osteomyelitis leads to an open sore that is draining pus, then its surrounding skin is at a higher risk of developing squamous cell cancer.
- Septic arthritis- Sometimes, infection within bones may also spread into any nearby joint.
- Impaired growth- Normal growth in bones or joints in children can get affected if the condition occurs in the softer areas, which are termed as growth plates, at either end of the long bones of the arms and legs.
Prevention
The best way to prevent this condition is cleanliness and tidiness. If you or your child is having a cut, especially a deep cut, it is important to wash it completely. Flush out any open wound under running water for a minimum of five minutes, after which you will need to bandage it in sterile bandages.
If you suffer from chronic osteomyelitis, then it is important to make sure your doctor is aware of your medical history. This will help you work together to keep the condition under control. If you are suffering from diabetes, then you will need to pay close attention to your feet and contact your doctor at the first sign of any infection.