Anal Fissure
Anal Fissure is a tear in the thin mucosa (moist tissue) that lines the anus. It occurs on passing large or hard stools during the bowel movement. Usually, the person may experience pain and bleeding with bowel movements due to Anal Fissures. At the end of the anus (anal sphincter), the person might also experience spasms in the ring of muscle. Although it affects people of any age, it is very common in infants. Some people need simpler treatments while others require medications and surgery for the same.
Causes of Anal Fissure
The causes of an Anal Fissure include:
- Straining and constipation during bowel movements
- Childbirth
- Passing hard or large stools
- Chronic diarrhea
- Crohn’s disease
- HIV
- Syphilis
- Inflammatory bowel disease
- Tuberculosis
- Anal cancer
Symptoms of Anal Fissure
The symptoms of the Anal fissure are:
- Blood on the stool after a bowel movement
- A skin tag on the skin or lump on the skin near the Anal fissure
- Pain during bowel movement that might sometimes be severe.
- Crack in the skin near the anus that is quite visible
- Pain lasting for hours after the bowel movements.
Diagnosis of Anal Fissure
Your doctor will note down your medical history while performing a physical examination including inspection of the anal region. The tear is mostly visible. Usually, this helps to diagnose an Anal Fissure. The acute Anal Fissure appears like a fresh tear while a chronic Anal fissure has a deeper tear. A chronic Anal fissure may have external or internal fleshy growths. If you have an Anal fissure for more than 8 weeks, then it is a Chronic Anal Fissure.
The location of the fissure may tell you about the cause. If there is a fissure on the side of the anal opening, then it is a sign of Crohn’s disease. Your doctor might recommend some other tests if he or she thinks that you are suffering from the condition.
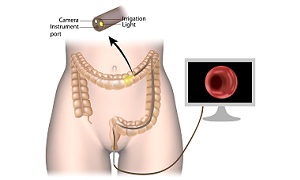
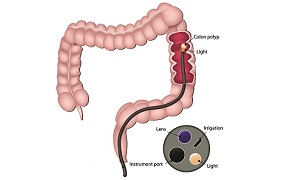
Colonoscopy
To inspect your colon, your doctor will insert a flexible tube into the rectum. If you are more than 50 years old or at a risk for colon cancer, you may need to undergo this test. Your doctor will recommend this test if you have diarrhea or abdominal pain.
Anoscopy:
Your doctor will insert a tubular device called anoscope into your anus to visualize the anus and the rectum.
Flexible sigmoidoscopy
Flexible sigmoidoscopy involves the insertion of a flexible, thin tube into the bottom of your colon with a tiny video. If you are under the age of 50 and do not experience any risk for colon cancer or intestinal diseases, you may need to undergo this test.
Treatment options for Anal Fissure
Non-surgical treatments
- Topical anesthetic creams: It includes lidocaine hydrochloride (Xylocaine) that helps in relieving the pain.
- Externally applied nitroglycerin (Rectiv): It helps in increasing blood flow to the fissure, helps relax the anal sphincter, and promotes healing. Nitroglycerin is the treatment of choice when other treatments fail. The side effects include a headache that might be severe.
- Blood pressure medications: It includes diltiazem (Cardizem) or oral nifedipine (Procardia) that helps to relax the sphincter. You can take these medications externally or orally. When nitroglycerin is ineffective or causes any side effects, you can apply these externally.
- Botulinum toxin type A (Botox) injection: It paralyzes the anal sphincter muscle and relieves the spasms.
Surgical treatments
If you are suffering from a chronic Anal fissure that does not heal by any other treatments, or if you have severe symptoms, you might need to undergo surgery. Your surgeon will perform Lateral Internal Sphincterotomy (LIS) in which he or she will cut a small portion of the anal sphincter muscle. This reduces pain and spasms that promotes healing. For the treatment of chronic fissure, surgery is the best treatment.
Changes in lifestyle
There are many lifestyle changes that you can do for relieving discomfort and to promote healing of the fissure. This also helps to prevent a recurrence.
- Drinking enough fluids: When you drink ample fluids, you can prevent constipation.
- Eat foods rich in fiber: Include about 30 grams of fiber per day in your diet to keep stools soft and to promote healing of the fissures. Foods rich in fiber are nuts, fruits, whole grains, and vegetables. Fiber supplements may also help you. Do not increase your fiber intake all of a sudden. A gradual increase prevents bloating and gas.
- Avoid straining: Straining during bowel movements can create pressure that causes a tear or open up a healing tear.